How research on newborns in West Africa led to the development of a tool in Canada that predicts a deadly condition in babies worldwide
Two babies are born minutes apart.
One is lethargic, has a fever and is breathing rapidly.
The other is alert, has a normal temperature, and is breathing regularly.
Both have sepsis. Both could die if the sepsis is left untreated.
That’s the challenge with neonatal sepsis. It is hard to detect, hard to diagnose and the longer you wait to treat it, the more life threatening it becomes.
Sepsis is an overwhelming response to an infection that spreads throughout the bloodstream. Normally the body uses its immune system to fight infection, but in sepsis, the immune response is impaired causing serious damage to tissues and organs.
Sepsis is particularly dangerous for babies because their immune systems are not fully developed, making it harder for them to fight off infections. A full recovery from neonatal sepsis is dependent on an early diagnosis and prompt treatment with antibiotics or antiviral medications.
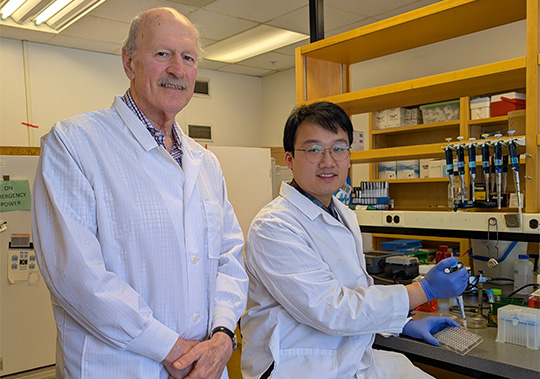
Sepsis is one of the leading causes of death in newborns in The Gambia. Microbiologist Dr. Bob Hancock and his lab at the University of British Columbia extracted RNA from blood cells collected from 700 babies in the West African country to find out why neonatal sepsis rates were so elevated. They sequenced the RNA to look for changes in gene expression linked to sepsis. Out of the 700 babies, they detected that 15 had sepsis in the first week of life.
“The Eureka was when we went back and looked at the babies, we saw big changes occurring at the time of birth in babies that were going to go on to acquire sepsis compared to babies who just had a local infection, or babies who didn't have any infection at all,” said Dr. Hancock. “In other words, sepsis was already starting, even though those babies looked healthy.”
The team used their findings to apply bioinformatics tools—software programs that analyze gene expression patterns in the blood of newborns—to identify specific molecular markers associated with sepsis. “So, we can predict sepsis before it occurs,” Dr. Hancock explained, “and that is astonishingly important because those babies can now be carefully monitored and treated as early as possible, rather than waiting until they're really getting sick.”
A relatively small number of babies born in Canada have sepsis—1 to 5 cases per 1,000 live births—but those that do can be born in rural or remote areas where getting rapid lab results is challenging. A predictive tool like the one Dr. Hancock’s lab developed could help physicians detect sepsis in newborns more quickly, averting long term health issues and even death.
CIHR recently awarded Dr. Hancock’s collaborators a grant to conduct clinical studies on a predictive tool for sepsis in the general population. The tool is integrated into a point-of-care device that enables physicians to predict sepsis at the patient’s bedside, accelerating treatment and improving chances of recovery.
“Sepsis is the cause of 20% of all deaths on the planet,” Dr. Hancock explained. “It’s also the cause of almost all the deaths from pandemics like COVID. It’s the number one cause of death in hospitals. So, it’s a big deal."
At a glance
Issue
Neonatal sepsis is the third major cause of death for babies 28 days or younger. It is difficult to diagnose sepsis in newborns and if not treated quickly it can cause developmental delays, learning disabilities and death.
Research
Dr. Bob Hancock and his team, including MD/PhD student Andy An at UBC and collaborator Dr. Amy Lee from Simon Fraser University, developed a software program that can predict sepsis in newborns, even in babies that do not have any symptoms of the condition.
- Date modified: